 About 1 in 4 women and 1 in 4 men die from heart disease and cardiologists often warn that there are some differences in symptoms experienced by women and men during a heart attack. The hallmark chest pain is more likely to be felt by men than women. Women may experience less obvious symptoms like trouble sleeping, nausea, fatigue and jaw pain. However, there is a lot of overlap in symptoms between men and women.
About 1 in 4 women and 1 in 4 men die from heart disease and cardiologists often warn that there are some differences in symptoms experienced by women and men during a heart attack. The hallmark chest pain is more likely to be felt by men than women. Women may experience less obvious symptoms like trouble sleeping, nausea, fatigue and jaw pain. However, there is a lot of overlap in symptoms between men and women.
To keep us alive, blood has to deliver oxygen and nutrients to our heart and other body organs but, with advancing age, plaques build up inside the walls of our heart arteries, also known as coronaries.
When these plaques grow large, they narrow the opening of the coronary arteries and doctors speak about coronary heart disease. This is the most common type of heart ailment and the leading cause of death in developed countries, responsible for approximately 20 percent of all deaths among men and women.
Symptoms in men
Coronary heart disease has no noticeable symptoms when the body is at rest. A partially occluded coronary artery can reduce the flow of blood to an area of heart muscle but, fortunately, heart areas have a number of different pathways for blood to reach them. There are three main heart arteries which encircle the heart like crowns (that is why they are called coronaries), while smaller blood vessels branch out from each of them and go to different parts of the heart.
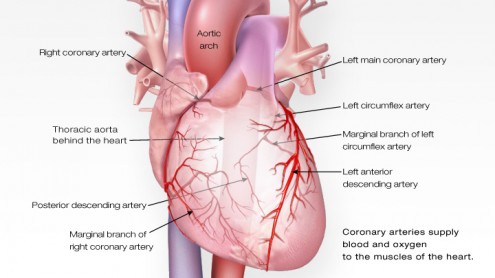 Thus, if one of the coronary arteries does not supply enough blood to a heart area, another can do so instead. Besides, when a coronary artery does become narrow, the small blood vessels around it grow larger to provide oxygen and nutrients. This process serves as an alternate route of blood supply and is known as collateral circulation.
Thus, if one of the coronary arteries does not supply enough blood to a heart area, another can do so instead. Besides, when a coronary artery does become narrow, the small blood vessels around it grow larger to provide oxygen and nutrients. This process serves as an alternate route of blood supply and is known as collateral circulation.
Yet a coronary artery may become so narrow that even with this help not enough oxygen can be delivered when patients exert themselves. This is called myocardial ischemia, meaning lack of blood for the heart muscle. The main symptom is pain due to insufficient oxygen reaching the heart. It is called angina pectoris and typically lasts for several minutes.
Angina is a heavy pressure beneath the breastbone but it may spread to the shoulders, back, neck, arms, jaw or teeth. When it occurs as a consequence of a large plaque in a coronary artery, it is called stable angina because the pain is predictable.
While some heart attacks are as sudden and intense as those spectacular collapses seen in movies, most of them start slowly, with only mild pain or discomfort. Often people affected are not sure what is happening to them and wait too long before getting help. Cold sweats, nausea, vomiting and other gastrointestinal symptoms are common. The victim may be dizzy or short of breath, seem pale or extremely anxious and have a heart rate that is rapid or irregular. There are also what are called salient heart attacks, where there is virtually no pain or other symptoms.
Common heart attack symptoms in men include:
- Pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw or back)
- A feeling of fullness, nausea, indigestion, heartburn or abdominal pain
- Shortness of breath
- Sweating or a cold sweat
- Feelings of anxiety or an impending sense of doom
- Fatigue
- Trouble sleeping
- Lightheadedness or dizziness
Note, however, that roughly 80 percent of people who have chest pain and discomfort are suffering from indigestion, acid reflux or another relatively benign condition.
Stable and unstable angina
Stable angina almost always comes after physical activity, emotional stress, exposure to cold or a heavy meal. Having sought medical advice after the first alarming experience of angina and been prescribed medication, patients learn to predict with reasonable accuracy when it is likely to recur. Taking a pill improves blood flow within minutes and makes the symptoms fade and disappear. Stable angina does not usually pose an immediate threat to life. Most deaths from coronary heart disease are actually caused by heart attacks and cardiac arrests (see below).
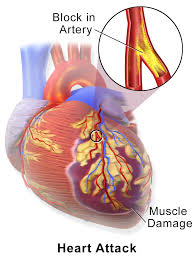
A heart attack, also called myocardial infarction, occurs when a plaque breaks up and blood coagulates to close the rupture this has caused in the wall of the artery. As with a superficial skin wound, the blood forms a small, solid mass called a clot or thrombus and doctors speak about coronary thrombosis. The clot is a pale yellowish color because it does not contain red cells. This little yellow bastard can severely restrict the blood flow in a coronary artery, causing an area of heart muscle to die. A pain may appear that can come and go for hours, called unstable angina, and there is an immediate threat to life.
The severity of a heart attack depends on how large the blockage is, how long the artery is occluded and the presence or absence of collateral circulation. If the damage to the heart muscle is extensive life suddenly ends, if it is moderate the heart will not be able to pump as effectively as before, and if it is minor life will continue normally but with possible consequences in the future due to the scar that has formed on the heart with the healing of the ruptured wall.
Symptoms in women
Coronary heart disease has been widely considered a “man’s disease”. It is true that it primarily affects men but it is also true that more women than men die of coronary heart disease each year in developed countries. Middle-aged men are about four times more likely to suffer from coronary heart disease than women of comparable age but after menopause the gap starts to close and by the eighth decade of life men are not at much more risk than women.
Eventually, each year, in absolute numbers, more women die from coronary heart disease than men, because more men are killed by accidents and lung cancer. Women with coronary heart disease have worse outcomes than men because atherosclerosis affects not only their coronary arteries but also the smaller vessels of their heart. This is probably the reason why women experience somewhat different symptoms from men during a heart attack.
The conventional wisdom is that men experience often crushing chest pain during a heart attack, while women may complain of pressure or pain in the lower chest or abdomen, which may spread to the shoulders or arms. Many women do not feel chest pain at all or feel the pain in the upper abdomen and back. A recent study found that one in five women aged 55 or younger may not experience any chest pain while having a heart attack.
Common heart attack symptoms in women include:
- Uncomfortable pressure, squeezing, fullness or pain in the center of your chest. It lasts more than a few minutes, or goes away and comes back.
- Pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath with or without chest discomfort.
- Other signs such as breaking out in a cold sweat, nausea or light headedness.
- As with men, women’s most common heart attack symptom is chest pain or discomfort. But women are somewhat more likely than men to experience some of the other common symptoms, particularly shortness of breath, nausea/vomiting and back or jaw pain.
Note that there is a lot of overlap in symptoms between men and women.
Cardiac arrest
Even though a heart attack can be lethal, many sudden deaths occur from what is called cardiac arrest. It is important to make a distinction between a heart attack and a cardiac arrest. Heart cells transmit a small pulse of electric current which makes the heart contract rhythmically to maintain the flow of blood.
This electrical current is sometimes interrupted and the rhythm of the heart becomes irregular, a condition known as arrhythmia. A cardiac arrest occurs when the heart develops a severely abnormal arrhythmia, called ventricular fibrillation, that causes the heart to flutter instead of beating. With no blood flow, the person just falls over and dies within few minutes. This is different from a heart attack, where the heart continues to beat but the flow of blood is blocked.
Nevertheless, most cardiac arrests are triggered by past heart attacks, even the salient ones, which have left a dysfunction in the heart’s system for supplying pulses of electric current.
Heart failure
Heart attacks can lead to another condition called heart failure, which has a very poor prognosis. In contrast to cardiac arrest, heart failure does not mean that the heart stops beating but rather that it fails to pump blood effectively. This can happen after a single heart attack that injures an area of heart muscle or from a series of small ischemic episodes which result in accumulating damage. In either case, the damage forces the heart to work harder to deliver blood, and as a result the heart muscle thickens and stretches. The over-exertion eventually causes the heart to weaken and results in heart failure.
Despite the confusing similarity in names, heart attack, cardiac arrest and heart failure are different conditions. But they are all mainly due to atherosclerosis.
Strokes
Another consequence of atherosclerosis is ischemic stroke, the brain equivalent to a heart attack. The coronaries are not the only arteries that can be narrowed by plaque. The same occurs, for example, in the two carotid arteries, which pass through the neck and supply blood to the brain. A clot that is formed in a carotid artery may reach the brain through the circulatory system and block a blood vessel. This causes brain cells to die and is called an ischemic stroke.
Another type of stroke can occur when a blood vessel in the brain bursts, and this is termed a hemorrhagic stroke. In most countries, ischemic strokes are much more common than the hemorrhagic variety but there are exceptions such as Japan.
Coronary heart disease, strokes and other heart disorders such as arrhythmias, infections and defects of the heart, arteries and veins come under an umbrella term called heart disease or cardiovascular disease. In developed countries, heart disease accounts for approximately four in ten deaths in both men and women.